Oral Bacterial DNA Testing
The Oral Microbiome and Periodontal Disease
There are 3 primary ways in which the mouth can deteriorate:
- Tooth decay
- Gum/bone (periodontal) disease
- Mechanical dysfunction
The first two are the result of a disruption in the healthy balance of the oral microbiome. Like the gut, the mouth is teeming with bacteria, both “good” and “bad”, and their balanced relationship is known as symbiosis. Disease ensues when the bad bacteria overpopulate and “crowd out” the good bacteria, creating a condition known as dysbiosis. The result of this dysbiosis can be very complex, and while the mouth as a whole can be considered as “diseased”, there are microcolonies and biofilms that are unique and distinctive, having different effects on different tissues based upon the type of bacteria they contain. For instance, while there are other bacterial strains implicated, we know that the major strain responsible for tooth decay is Streptococcus mutans. The establishment and overpopulation of this bacteria can occur in the deep grooves on the top chewing surfaces of posterior teeth, between the teeth, and at gum/tooth interface. These bacteria feed on carbs (particularly simple carbs like “sugar”, and even fruit) and create acid as a by-product, and it’s the acid that dissolves away the enamel, allowing bacteria to reach the softer more decay-prone dentin layer. Periodontal (gum/bone) disease is the result of more complex biofilms that form below the gums. The progression of this disease is the result of both direct and indirect mechanisms... or in other words, the disease progresses from the direct action of the bacteria present in the biofilm and the host (immune) response. Your major immune defense against periodontal disease is your saliva, so reduced salivary flow or saliva that lacks certain minerals, enzymes, or immunoglobulins can allow these harmful biofilms to take hold.


While there are a number of local and systemic factors that can contribute to periodontal disease, a short list may include:
- Poor oral hygiene
- Poor diet (highly processed; sugars)
- Stress
- Crooked or crowded teeth
- Underlying immunodeficiencies
- Genetic mutations
- Toxins that interfere with our normal immune response or tissue/bone turnover
- A damaged gut (gut dysbiosis)
- Mouth breathing
- Defective and failing dental work
- Dry mouth (medication side effects; autoimmune disorders)
- Hormonal changes (particularly during pregnancy)
- Oral contraceptives
- Smoking
- Diabetes
Traditional means of diagnosing periodontal disease is done by intra-oral evaluation, x-rays, periodontal charting, and longitudinal observation of those results. With this approach, many years may pass before ever observing changes, during which time silent destruction can result. Alternatively, modern-day DNA techniques allow us to sample the oral microbiome and to detect these changes before chronic disease takes a foothold.
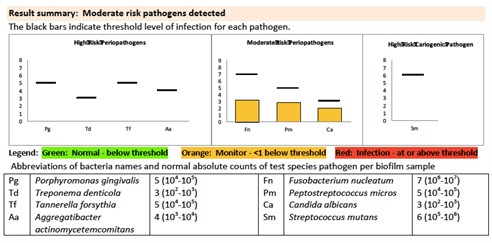
The examples below show bacterial DNA test results of two different patients. The first patient presents with concerning results, with high levels of “moderate risk” bacteria and moderate levels of “high risk” (more destructive) bacteria. This is not a very common test result, and is the most challenging to treat. In addition to an intensive oral approach (as described below), connecting with an integrative health practictioner, functional medicine doctor, or naturopath will be necessary to address systemic issues that may be contributing to this oral presentation.
Bacterial DNA Results
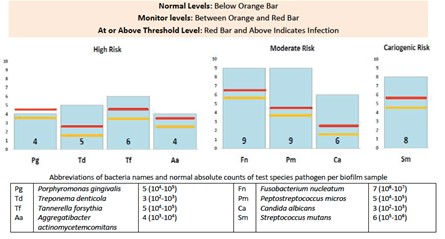
The bacterial DNA results shown next represent a milder state of periodontal disease. It is possible this condition can be corrected with less extensive forms of mitigation, like diet modification, oral hygiene coaching, increased frequency of cleanings, and the introduction of new hygiene products (as discussed below).
Regardless of the form of treatment, it is important to realize that in order to successfully treat periodontal disease, we need to achieve and maintain both a balanced oral microbiome AND a robust immune response... or put another way, we need to address both the local and systemic contributing factors. First, we will discuss addressing the oral environment.
Regardless of the form of treatment, it is important to realize that in order to successfully treat periodontal disease, we need to achieve and maintain both a balanced oral microbiome AND a robust immune response... or put another way, we need to address both the local and systemic contributing factors. This requires a collaboration between us and your functional, integrative, or naturopathic practitioner. In the event you do not have one of these health partners, we can recommend one to you.
Diet Modification
The very first step of returning the mouth to a healthy state is assessing and potentially modifying your diet. Best to avoid:
- Sugars, particularly added sugars (read food labels, sugar is everywhere!). Fruit also contains sugars that feed harmful bacteria, fruit juices being worse that whole fruit.
- Highly processed foods
- Frequent snacking
- Carbonated beverages (create an acidic mouth)
Oral Hygiene
The idea is to break up the biofilm that forms between the teeth, below the gums, and in the concavities and irregularities of the root surfaces of the teeth. At minimum, brushing and flossing twice a day is crucial, after every meal is best (three times a day). A WaterPik is very effective if used morning and night. You can add all-natural mouthwashes and certain oils, like grapefruit seed extract, and grape seed extract (both known to kill harmful bacteria), to the reservoir. The use of Proxabrushes or Soft-Picks (both made by GUM brand) is also highly effective in disrupting the biofilm. There are also a number of other beneficial products that we recommend, which is available as a handout to our patients.

Mechanical Debridement
The foundation of all periodontal therapy is scaling and root planing (“deep cleaning”), which is the mechanical debridement of the calcified biofilm (aka tartar) beneath the gums. The number and frequency of these sessions depends upon your particular microbiome.
Ozone Rinses
BioSure is a company that makes high quality at-home products that can create ozone water within 3 minutes time using only tap water. Ozone is a powerful antioxidant form of oxygen, much more effective at killing bacteria (along with viruses and fungi) than other chemicals, and completely safe with zero side effects. Ask us about BioSure ozone canisters.
Probiotic Lozenge
After completing the antibiotic rinse regimen, introduce beneficial bacteria in the form of oral probiotic lozenges. We recommend either Great Oral Health or Hyperbiotics Pro-Dental. This should be continued indefinitely.
Re-Testing
Re-testing is essential to understanding your particular response to the treatment approach. It is important to realize that though the results of this test will show some improvement, the amount of improvement will vary from person to person and is dependent upon a number of factors. Since the mouth is not a sterile environment, it is likely that there will still be some, albeit much lower, levels of harmful bacteria present. While it is possible to obtain test results that show no detectable levels of these harmful bacteria, the goal should be progress, not complete and immediate resolution. Periodontal disease is a chronic condition, and therefore requires dedication and commitment on the part of both you and our dental team.
The best chances you will have at achieving and maintaining a healthy mouth will rely on you becoming obsessed with cleaning, eating well, and coming in for frequent cleanings. It would be beneficial to periodically re-test (every 1-3 years) to ensure there hasn’t been a relapse to a diseased state. If disease returns, despite having addressed all of the local (oral) factors and despite you having strictly adhered to our recommendations, it is possible there are systemic factors at play. In this case we highly recommend you establish a relationship with an integrative or functional health practitioner who can thoroughly evaluate your current health state on a cellular level, to determine if there are other toxins, hidden infections, or genetic abnormalities present that could be interfering with the normal function of your immune response. (Please ask us if you’d like a recommendation).
The Oral/Systemic Connection
Until recently, the bacteria associated with periodontal disease were thought to only reside in the mouth. Evidence now overwhelmingly supports the idea that these bacteria can and do get into the blood stream, traveling to other parts of the body, and cause disease at distant sites. For example, Porphyromonas gingivalis, which is known to be an incredibly destructive bacteria associated with periodontal disease, is also being found in the brain tissues of dementia patients 1, or in the blood clots of heart attack victums 2. Fusobacterium nucleatum, another periodontal pathogen, has a strong connection with colorectal cancer 3. While the cause-and-effect relationship is still being studied, it makes sense that we should eliminate these overgrowths, wherever they reside. This is why we recommend establishing a relationship with an integrative or functional health practitioner, who can evaluate your health on a cellular level, as well as the gut microbiome.
Seymour T, Zhang J. Porphyromonas Gingivalis in the Pathogenesis of Alzheimer’s Disease and Its Therapeutic Target. Journal of Exploratory Research in Pharmacology 2022;7(1):45-53
Zhang J, Xie M, Huang X, Chen G, Yin Y, Lu X, Feng G, Yu R, Chen L. The Effects of Porphyromonas gingivalis on Atherosclerosis-Related Cells. Front Immunol. 2021 Dec 23;12:766560. doi: 10.3389/fimmu.2021.766560. PMID: 35003080; PMCID: PMC8734595.
Ni Wang, Jing-Yuan Fang, Fusobacterium nucleatum, a key pathogenic factor and microbial biomarker for colorectal cancer. Trends in Microbiology, Volume 31, Issue 2, 2023, Pages 159-172.
Our Commitment
Be assured that we are continually evolving and improving our treatment recommendations based upon the latest research, so if new treatment options become available that fit within our health-oriented approach, you will certainly be notified. And as always, it is important to us that you are educated about your existing state, how that relates to a healthy state, your treatment options to return to a healthy state, and the risks and benefits of those options... so please do not hesitate to ask questions.
Sincerely,
LeBlanc Dental